De-mystifying lower back pain
We have been getting a lot of Telehealth consultations this week from clients complaining about lower back pain! Whether or not it was due to the increased stress associated with isolation, social distancing, working at a less-than-ideal home office, or lifting their child out of their car seat that caused your back pain! So, I thought I can demystify lower back pain for you, so that you know how you can self-manage at home, or when to seek professional guidance from your physiotherapist.
What is low back pain?
Low back pain is an umbrella term!
It’s a symptom rather than a disease and can result from several different known or unknown abnormalities or injury. Some discomfort can come on suddenly while you were doing something, or some build up gradually over time.
Lower back pain is commonly accompanied by pain in one or both legs. Some people with low back pain also have associated altered sensations in their legs, such as tingling. Low back pain is usually non-specific; this means that the pain cannot be attributed to just one cause but rather a combination of different factors (joint stiffness, age-related bony changes, nerve compression) – this accounts for 90% of people with low back pain.
Myth 1: I need a scan for my lower back
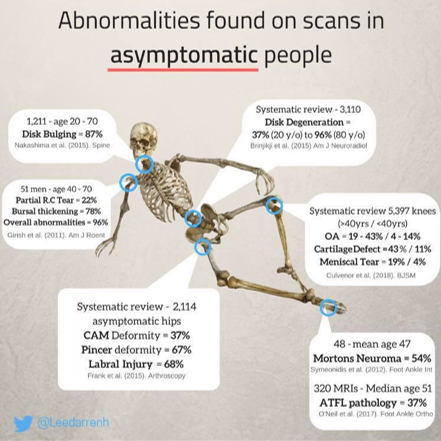
Many sufferers of low back pain receive routine spinal imaging (CT, MRI) despite evidence-based recommendations that ONLY call for imaging in people with worsening symptoms or neurological deficits. For example, those who lose feeling or strength in their legs, or lose control of their bowel or bladder.
We often hear clients say: “I did an MRI/X-Ray recently and they found that I have degeneration of my spinal segments, or “I have a bulging disc” and it leads to the assumption that something’s damaged, or that something is “out of place”. This tends to cause a ripple effect, where people believe they need a “fix” a problem that has been identified on scans.
In fact, many high-level studies have shown that there is a poor correlation between imaging results and symptoms. AKA what shows up in the scan might not be the cause of your pain AT ALL. Or, you can be in significant pain, but your spine looks ‘normal’. Where does that leave you?
Although there are specific pathological causes (disc degeneration & spondylolisthesis) associated with an increased risk of lower back pain, no evidence exists that imaging improves patient outcomes. On the contrary, scans may lead to poorer health outcomes, greater disability and work absence due to ‘pathologising’ the problem! In reality imaging should be used to rule out serious conditions only, rather than “fishing” for a diagnosis.
Myth 2: Pain means I’m damaging something!
Pain is multi-factorial! Factors such as circumstances, previous pain experiences and coping styles all affect the way we perceive pain.
Pain is a protector – by making unpleasant feelings, your brain changes your behaviour in order to “avoid” injury to allow tissue to heal. Usually, a stimulus – the pain perception – is relayed to your brain, which then regulates the level of your response – the pain reaction. During injury however, this process is enhanced. This may cause a higher-than-usual pain reaction to the same amount of pain perception. Therefore people with similar back issues can experience pain very differently – it not just a matter of “high pain threshold”!
Myth 3: “Slipped disc”
The term “slipped disc” often causes many to visualise a portion of the spine dislocating in the body. In fact, the medical term “slipped” isn’t remotely accurate to what happens. Each disc has two portions: the harder outer ring, and a gelatinous inner portion. When a disc “slips” or herniates, the gelatinous inner portion pushes into the tougher outer ring, causing pain and discomfort.
Sometimes, it may rub into your spinal nerves and cause inflammation of the nerve, leading to numbness and pain along the nerve. However, because the spinal column is a small space with an intricate network of blood and nerves, an inflamed disc can place extra pressure on the surrounding structures such as soft tissues, muscles, nerves & ligaments without trying too hard.
Depending on the degree of herniation, it may dictate the symptoms experienced, and time taken to recover. Symptoms are usually short-lived as the localised response settles down, and the body becomes accustomed with the shift of the disc. Thank goodness! Studies have shown that discs are reabsorbed into the body in six to eight months, but symptoms can be as short as two days!
Myth 4: I need surgery!
Renowned physiotherapist Peter O’Sullivan said in a recent interview that:
“For someone without private health insurance, it would be cheaper for someone to go through the public system and have spinal surgery, than to see a physiotherapist for a course of education and progressive exercise”.
That in itself sounds ridiculous! Think about it…
The primary rationale for surgery is that it will relieve root irritation or compression, and in turn, lead to less pain. However, several studies comparing surgery & conservative management (physiotherapy) have found that:
• Benefits of conservative management is equal to surgical intervention in terms of pain, symptoms and quality of life.
• No reduction in sciatica (nerve pain down the back of your leg) or improved quality of life between the two groups.
• In disc-herniation surgical studies versus conservative management, pain is relieved earlier in surgical groups, but were no different at 12 weeks later between the groups.
Emerging evidence suggesting a conservative approach to management of lower back pain as the primary course of treatment because patients tend to improve with or without surgery. This does not say that surgery is not at all required. Patients who continue to have debilitating or progressive neurological deficits despite initial physiotherapy management may need a referral to a surgeon.
Myth 5: Now that I have back pain, I’ll have it forever
If you have acute low back pain you need to be aware that your pain levels will take time to decrease when engaging in your individualised exercises and is not immediate. Recovery and pain actually take longer with complete rest and inactivity. So, keep moving people!
You can usually recover from back pain within a few weeks and continue to improve over a few months. Recurrences of low back pain are also common, with evidence showing that 33% of people will have a recurrence within a year after you recovered. Unfortunately, 10-15% develop chronic low back pain, with 78% suffering from relapses. However, chronic low back pain is often seen to be attributed to factors that may be work-related, related to personal/family issues and/or psychological health.
While it is tempting to refrain from all physical activity while you’re experiencing pain or discomfort from your back, this can lead to higher levels of pain, greater disability and poorer recovery. Furthermore, movement prevents maladaptive movements (such as avoidance behaviours) which may be detrimental in the long term. Instead, try to remain as active as possible with low impact activities such as walking or gentle stretching.
The Reload Team: Our role as physiotherapists is simple:
• Relieve the pain. Manual therapy in the acute & subacute phases allows us to restore mobility in stiffer joints and reduce muscular tension. It also opens a window of opportunity to allow for more movement. Manual handling will be limited due to the current pandemic, however self release work at home is invaluable and we will give you clear instructions on how to do so safely.
• Regain the movement. Exercise prescription and guidance to ensure you’re performing the movements correctly and progressing them appropriately. Immobility/reduced movement often leads to poorer outcomes, so it is imperative that we normalise movement behaviours as soon as possible!
• Reload for resilience! Become stronger than when you started!
At Reload Physio we recognise that there is no “one size fits all” exercise protocol, but we aim to create one that is both individualised & achievable for you. Having the appropriate equipment for strength & conditioning, and movement control allows us to tailor a program together.
If you would like more information, please get in touch by phoning our lovely reception staff, or booking yourself in for a Telehealth consultation.
We are currently offering free 15 minute phone consultations if you have any questions instead of our usual injury screening appointments.