Staying Strong as Footy Seasons Kick Off
As we move into late summer and early autumn, many athletes are shifting gears toward pre-season training for AFL and NRL. This is a phase where training volume, speed work, and (for contact sports) tackling gradually increase.
As we move into late summer and early autumn, many athletes are shifting gears toward pre-season training for AFL and NRL. This is a phase where training volume, speed work, and (for contact sports) tackling gradually increase. From a physio’s perspective, this period isn’t something to fear — but it does benefit from smart preparation and good load management.
Across both Australian football and rugby league, injury surveillance data shows that the most common issues are muscle strains, joint sprains, and impact-related injuries, rather than sudden or severe injuries. In AFL, hamstring strains consistently remain the most frequently reported time-loss injury across seasons, largely due to the high-speed running and sprint demands of the game (Saw et al., 2018; AFL Injury Report, 2022). The good news is that most hamstring injuries are mild to moderate and respond well to appropriate strength-based rehabilitation and progressive loading.
Groin and hip-related pain is also commonly seen early in the season, particularly as kicking volume, cutting, and change-of-direction drills increase. Research suggests these injuries are often associated with changes in training load rather than a single incident, highlighting the importance of gradual exposure rather than resting away from activity altogether (Mosler et al., 2015).
In the NRL, the physical nature of the game plays a larger role. Muscle strains and ligament sprains around the knee and ankle are frequently reported, often linked to tackling or awkward landings (Gabbett, 2010). Shoulder injuries, including minor instability episodes, are also common due to contact, but most are well managed with early assessment and structured rehabilitation.
Concussion remains an important focus in both AFL and NRL. Current evidence shows that most athletes recover well when concussion is recognised early and managed appropriately, using graded return-to-play protocols rather than prolonged rest or fear-based restrictions (McCrory et al., 2017).
What the evidence consistently shows is that injury risk is influenced by preparation, workload progression, and recovery, not simply the sport itself. Gradual increases in training load, regular strength training, good sleep, and early management of niggles are all associated with reduced time lost to injury.
From a physiotherapy perspective, pre-season is an opportunity. It’s the ideal time to address strength deficits, improve movement efficiency, and build resilience so the body is better prepared for the demands of the season ahead.
If you’re gearing up for AFL, NRL, or local competition, now is a great time to visit a physiotherapy clinic or contact your physio. A pre-season assessment or tailored strength program can help you train with confidence and stay on the field longer.
References
AFL Injury Report. (2022). AFL injury report: Season 2022. AFL. https://www.afl.com.au/news/1211880/afl-and-aflw-injury-reports
Gabbett, T. J. (2010). The development and application of an injury prediction model for noncontact, soft-tissue injuries in elite collision sport athletes. Journal of Strength and Conditioning Research, 24(10), 2593–2603. https://doi.org/10.1519/JSC.0b013e3181f19da4
McCrory, P., Meeuwisse, W., Dvořák, J., Aubry, M., Bailes, J., Broglio, S., Cantu, R. C., Cassidy, D., Echemendia, R. J., Castellani, R. J., Davis, G. A., Ellenbogen, R., Emery, C., Engebretsen, L., Feddermann-Demont, N., Giza, C. C., Guskiewicz, K. M., Herring, S., Iverson, G. L., … Vos, P. E. (2017). Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. British Journal of Sports Medicine, 51(11), 838–847. https://doi.org/10.1136/bjsports-2017-097699
Mosler, A. B., Agricola, R., Weir, A., Hölmich, P., & Crossley, K. M. (2015). Which factors differentiate athletes with hip/groin pain from those without? A systematic review with meta-analysis. British Journal of Sports Medicine, 49(12), 810. https://doi.org/10.1136/bjsports-2015-094602
Saw, R., Finch, C. F., Samra, D., Baquie, P., Cardoso, T., Hope, D., & Orchard, J. W. (2018). Injuries in Australian Rules Football: An overview of injury rates, patterns, and mechanisms across all levels of play. Sports Health, 10(3), 208–216. https://doi.org/10.1177/1941738117726070
The Advantages of Youth Weightlifting
Author: Ben Lane. Weightlifting can be a valuable addition to a teenager's fitness routine when approached sensibly and with expert guidance. As professionals, we aim to educate, personalise programs, and promote safe practices for long-term health. The cumulative evidence unequivocally advocates for the inclusion of weightlifting in young athletes' training programs - 3 minute read.
In recent years, there's been a surge of interest in weightlifting among children and teenagers, fuelled by the desire to boost health, enhance sports performance, and foster positive self-perception among young athletes. A deep dive into various studies, including observational, correlational, and longitudinal data, sheds light on the myriad advantages of incorporating weightlifting into strength and conditioning programs. The impact is far-reaching, encompassing both physical and mental realms. This integration stands as a robust strategy, effectively reducing injury risks, enhancing strength, refining body composition, improving motor control, and bolstering bone mineral density. Moreover, weightlifting seems to wield psychological benefits, improving long-term health, cognitive function, fostering better health behaviours, and instigating positive social and psychological effects.
While concerns previously swirled around the suitability of weightlifting for young athletes due to hormonal considerations, recent literature challenges these notions. Instead, coaches are encouraged to implement weightlifting as the benefits far outweigh any potential risks for young athletes. Engaging in weightlifting exercises leads to significant improvements across various fitness domains, encompassing body composition, cardiovascular measures, motor fitness, and weightlifting performance. Under careful guidance, a window exists for strength and power gains with minimal risk of injury.
Youth weightlifting extends beyond performance enhancements; it emerges as a potent tool for injury prevention across diverse sports and activities, potentially reducing the occurrence of injuries by a significant margin. Studies showcase adaptations in bones, ligaments, and tendons, advocating for its inclusion in the training regimens of young athletes, making them more resilient to sports-related impacts. Aligned with lower limb movement patterns, weightlifting holds promise in transferring its benefits to critical sporting movements, contributing significantly to strength, power, and injury resilience.
Addressing apprehensions regarding bone development, expert consensus and studies emphasize the positive impacts of appropriately coached weightlifting programs. These programs foster bone formation and density in young athletes. Early engagement in weightlifting appears instrumental in laying the foundation for achieving peak musculoskeletal strength and potentially reducing overuse injuries in adulthood.
Considerations and Guidance:
Proper Supervision: Ensuring trained supervision is crucial during weightlifting sessions.
Personalization Matters: Tailoring workouts to individual capacities is key for safety and effectiveness.
Rest and Recovery: Emphasizing adequate rest and recovery between sessions is vital for injury prevention and muscle recovery.
Safety Insights:
Growth Plate Myth: Properly supervised lifting doesn't harm growth plates.
Reduced Risks: Focus on technique and gradual progression to minimize the risk of injuries.
Conclusion:
Weightlifting can be a valuable addition to a teenager's fitness routine when approached sensibly and with expert guidance. As professionals, we aim to educate, personalise programs, and promote safe practices for long-term health. The cumulative evidence unequivocally advocates for the inclusion of weightlifting in young athletes' training programs.
Contact any physiotherapist at Reload Physio for further information!
Stay informed, stay strong!
Resources
Harries, S. K., Lubans, D. R., & Callister, R. (2012). Resistance training to improve power and sports performance in adolescent athletes: a systematic review and meta-analysis. Journal of science and medicine in sport, 15(6), 532-540
Pichardo, A. W., Oliver, J. L., Harrison, C. B., Maulder, P. S., Lloyd, R. S., & Kandoi, R. (2021). Effects of combined resistance training and weightlifting on injury risk factors and resistance training skill of adolescent males. Journal of Strength and Conditioning Research, 35(12), 3370-3377
WOODS, B. (2019). Youth Weightlifting-A Review on The Risks, Benefits, And Long-Term Athlete Development Associated with Weightlifting Amongst Youth Athletes. Journal of Australian Strength and Conditioning, 27(3), 53-68
Conditioning for Life: How Exercise Physiology Enhances Long-Term Well-Being
How Exercise Physiology Enhances Long-Term Well-Being- A Blog post by Lily Beechey.
We will be delving into the realm of health and wellness, exploring how the guidance of an Exercise Physiologist becomes a beacon towards long-term well-being.
In today's blog post by Lily Beechey, we will be delving into the realm of health and wellness, exploring how the guidance of an Exercise Physiologist becomes a beacon towards long-term well-being. Beyond the realms of conventional fitness, these professionals delve into the intricate science of the body in motion, crafting personalised journeys that extend far beyond the confines of a single workout. Let's unravel how the expertise of an exercise physiologist becomes a cornerstone for a lifetime of holistic health.
The Exercise Physiologist Advantage
Tailored Wellness Plans:
An Exercise Physiologist isn't just a fitness instructor; they are navigators of wellness. Through comprehensive assessments and an in-depth understanding of your physiology, Exercise Physiologists design individualised wellness plans that align with your unique needs, goals and health considerations.
Continuous Monitoring and Adjustment:
Unlike generic workout programs, Exercise Physiologists provide ongoing support. Regular assessments and adjustments to your fitness plan ensure that it evolves with you, adapting to changes in your health, lifestyle and fitness levels.
Educational Empowerment:
One of the unique strengths of Exercise Physiologists lies in their commitment to education. By imparting knowledge about the intricacies of exercise and its impact on the body, they empower individuals to make informed decisions about their health, fostering a sense of ownership over their well-being.
Unlocking the Benefits of Exercise Physiology
Sustainable Fitness Habits:
Guided by an Exercise Physiologist, individuals cultivate sustainable fitness habits that transcend short-term goals. This shift from sporadic workouts to a consistent, tailored routine lays the groundwork for a lifelong commitment to health.
Injury Prevention and Resilience:
Exercise physiologists specialise in injury prevention. By identifying and addressing imbalances, weaknesses and potential risk factors, they guide clients in building resilience, ensuring a future free from the setbacks of injuries.
Optimising Aging Processes:
Collaborating with an Exercise Physiologist facilitates the optimisation of the aging process. Tailored exercise plans support cognitive function, maintain bone density and enhance cardiovascular health, enabling individuals to age with vitality and grace.
Chronic Disease Management:
For those managing chronic conditions, Exercise Physiology becomes a crucial ally. Integrating exercise into the treatment plan, under the guidance of a professional, enhances overall health and contributes to the effective management of various chronic diseases.
Enhanced Mental Well-Being:
Exercise is a powerful tool for mental well-being and exercise physiologists understand this connection deeply. Beyond the physical benefits, their guidance promotes mental resilience, stress reduction and a positive mindset that extends well beyond the confines of a workout session.
Your Journey to Lifelong Well-Being
Embracing the expertise of an exercise physiologist marks the beginning of a transformative journey towards lifelong well-being. Beyond the initial sessions, beyond the sweat and exertion, lies a future where health is not just a goal but a sustained reality.
Are you ready to embark on a personalised wellness journey? If you seek expertise and guidance tailored to your unique needs, then you're in the right place. Exercise Physiologist Lily Beechey will be offering her services at Reload Physio starting from early January 2024. Whether you're aiming to manage chronic conditions, prevent injuries, optimise your fitness, or simply enhance your overall well-being, Lily is here to guide you.
Prioritize your recovery: The power of sleep
Injured and on the road to recovery? Here's why sleep is a game-changer in injury management and how to optimise it with some smart sleep habits
Sleep and sleep hygiene play a crucial role in the management of injuries and the overall process of recovery. In this blog post we will investigate key reasons as to why sleep is important in injury management and recovery, as well as how good sleep hygiene practices can enhance these processes:
Tissue Repair and Growth: During deep sleep, the body releases growth hormone, which is essential for repairing and rebuilding tissues, including muscles, tendons, and ligaments. This is critical for the healing process after an injury.
Inflammation Reduction: Adequate sleep helps regulate the body's inflammatory response. Chronic inflammation can delay healing and exacerbate pain, so reducing inflammation through sleep is beneficial for recovery.
Immune Function: Sleep is closely linked to immune function. A well-rested immune system is better equipped to fight off infections and assist in the healing process, especially if an injury increases the risk of infection.
Pain Management: Sleep is a natural painkiller. It can reduce pain perception and improve the body's ability to tolerate discomfort. This can be particularly helpful for individuals recovering from surgeries or dealing with chronic pain due to injuries.
Mental Health and Coping:
Coping with an injury can be mentally taxing. Sleep plays a vital role in emotional regulation and can help individuals manage stress, anxiety, and depression, which are common emotional responses to injuries.
Memory Consolidation:
Sleep is essential for consolidating memories and learning. This can be valuable for patients who are undergoing rehabilitation and need to retain and apply new information about their injury, treatment plan, and exercises.
Energy and Physical Performance: Adequate sleep is necessary to restore energy levels and support physical performance. Individuals recovering from injuries may require extra energy to facilitate rehabilitation exercises and mobility.
To optimise the benefits of sleep for injury management and recovery, it's important to practice good sleep hygiene:
Consistent Schedule: Go to bed and wake up at the same time every day, even on weekends.
Create a Comfortable Sleep Environment: Ensure your bedroom is dark, quiet, and at a comfortable temperature. Invest in a good mattress and pillows.
Limit Stimulants: Avoid caffeine in the hours leading up to bedtime.
Technology Use: Reduce screen time before bed, as the blue light emitted by phones and computers can interfere with sleep.
Physical Activity: Regular exercise can promote better sleep but avoid vigorous exercise close to bedtime.
Limit Food and Alcohol: Avoid large meals and alcohol before bedtime, as they can disrupt sleep.
Relaxation Techniques: Practice relaxation techniques such as deep breathing, meditation, or yoga to reduce stress and promote better sleep.
Limit Naps: If you need to nap, keep them short (20-30 minutes) and earlier in the day to avoid interfering with nigh time sleep.
In summary, sleep is a critical component of injury management and recovery. It aids in tissue repair, inflammation reduction, immune function, pain management, mental health, and overall well-being. By practicing good sleep hygiene, individuals can maximize the benefits of sleep during their recovery process.
Smart Off-Season Training: A Game-Changer for Injury Prevention during the Season Elevate Your Performance, Safeguard Your Season!
In this blog post, we will explore the differences between these two methods and help you determine which one is best suited for you!
Greetings, Athletes and Sports Enthusiasts!
Welcome to another edition of our newsletter, where we're about to delve into a topic that could be the key to taking your game to the next level: the importance of strength training in the off-season to reduce injuries during the season. Whether you're a professional athlete or a dedicated sports enthusiast, understanding the role of off-season strength training in keeping you injury-free during the grind of the season is absolutely crucial. So, let's lace up our knowledge sneakers and explore why hitting the gym during the off-season is a strategy you can't afford to ignore!
1. Laying the Foundation for Resilience:
Picture your body as the ultimate athletic machine. Just as you'd tune up your car before a long journey, your body requires preparation before the demands of the sports season hit full throttle. Off-season strength training is your toolkit for building a robust foundation. By focusing on exercises that target muscle imbalances, flexibility, and core stability, you're setting the stage for optimal performance and injury prevention.
2. Addressing the Weak Links:
We're only as strong as our weakest link, and the same holds true for our bodies. Often, injuries occur when one area of the body is disproportionately weaker than the rest. Off-season training allows you to address these vulnerabilities head-on. By targeting muscles and movements specific to your sport, you're improving overall biomechanics and reducing the risk of overuse injuries that can plague your season.
3. Balancing the Load:
In-season practices and games are intense. They place high demands on certain muscle groups, leading to imbalances and overuse injuries. Off-season strength training gives you the opportunity to restore balance by working on opposing muscle groups and performing functional exercises that mimic the demands of your sport. This balance is your armour against injuries caused by muscular imbalances.
4. Enhancing Proprioception and Kinaesthetic Awareness:
Off-season training isn't just about lifting heavy weights. It's about enhancing your body's awareness and responsiveness. Incorporating exercises that challenge balance, coordination, and proprioception—such as stability ball exercises and single-leg movements—improves your body's ability to react effectively during the unpredictable moments of your sport, reducing the risk of awkward falls and sudden injuries.
5. Active Recovery and Injury Rehabilitation:
Injuries are often the result of accumulated stress on the body. The off-season provides a golden opportunity for active recovery and targeted injury rehabilitation. Engaging in strength training with lighter loads and focusing on controlled movements helps in rehabilitating minor injuries and ensuring that your body enters the season in top form.
6. Mental Resilience:
Physical training isn't just about the body; it's also about the mind. The discipline and commitment you demonstrate during the off-season translate into mental toughness during the season. Knowing that you've put in the effort to prevent injuries through intelligent training boosts your confidence and allows you to focus on the game itself. Off-season strength training isn't a detour; it's a direct path to peak performance and injury resilience. Think of it as an investment in your body's longevity and your sports journey's success. Remember, consult with a qualified physiotherapist to design a program tailored to your sport and individual needs. Here's to a season marked by strength, resilience, and triumph!
Wishing you a successful and injury-free journey, from the team at Reload Physio.
Gabbett, T. J. (2016). "The training—injury prevention paradox: Should athletes be training smarter and harder?" British Journal of Sports Medicine, 50(5), 273-280.
Hägglund, M., & Ekstrand, J. (2009). "A prospective study of injury incidence and injury patterns in a men's professional football league." European Journal of Sports Science, 9(4), 269-275.
Myer, G. D., Faigenbaum, A. D., Chu, D. A., Falkel, J., & Ford, K. R. (2011). "Rationale and clinical techniques for anterior cruciate ligament injury prevention among female athletes." Journal of Athletic Training, 46(4), 471-475.
Hewett, T. E., Myer, G. D., Ford, K. R., Heidt Jr, R. S., Colosimo, A. J., McLean, S. G., ... & Succop, P. (2005). "Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study." The American Journal of Sports Medicine, 33(4), 492-501.
Sugimoto, D., Myer, G. D., Bush, H. M., & Hewett, T. E. (2015). "Effects of compliance on trunk and hip integrative neuromuscular training on hip abductor strength in female athletes." Journal of Strength and Conditioning Research, 29(9), 2397-2406.
Silvers-Granelli, H. J., Bizzini, M., Arundale, A., Mandelbaum, B. R., & Snyder-Mackler, L. (2017). "Does the FIFA 11+ injury prevention program reduce the incidence of ACL injury in male soccer players?" Clinical Orthopaedics and Related Research, 475(10), 2447-2455.
Anderson, L., Triplett-McBride, T., Foster, C., & Doberstein, S. (2003). "Impact of training patterns on incidence of illness and injury during a women's collegiate basketball season." The Journal of Strength & Conditioning Research, 17(4), 734-738.
Faigenbaum, A. D., Farrell, A., Fabiano, M., Radler, T., Naclerio, F., Ratamess, N. A., ... & Kang, J. (2011). "Effects of integrative neuromuscular training on fitness performance in children." Pediatric Exercise Science, 23(4), 573-584
Dynamic vs. Static Warm-Ups: Which is Best Before You Exercise?
In this blog post, we will explore the differences between these two methods and help you determine which one is best suited for you!
Before diving into any physical activity, warming up your body is essential to prepare your muscles, joints, and cardiovascular system for the upcoming challenge. Warm-ups can help reduce the risk of injury, enhance your performance and improve your workout effectiveness.
When it comes to warming up, there are two primary approaches: dynamic and static warm-ups. In this blog post, we will explore the differences between these two methods and help you determine which one is best suited for you!
Let’s start with Dynamic Warm Ups Dynamic warm-ups involve performing movements that mimic the exercises you'll be doing during activity. These movements are done in a controlled manner and gradually increase in intensity to raise your body temperature and stimulate your muscles. Dynamic warm-ups typically involve active stretching, mobility exercises, and light aerobic activities. Here are a few of the key benefits they provide:
Firstly, they improve your joint range of motion! Dynamic movements take your joints and muscles through a full range of motion, promoting flexibility and mobility. This can be particularly beneficial for activities that require a wide range of motion, such as gymnastic sports, weightlifting, or high-intensity interval training (HIIT).
Secondly, Dynamic Warm Ups enhance Blood Flow: The active nature of dynamic warm-ups increases blood circulation, delivering oxygen and nutrients to your muscles. This helps to optimize muscle performance and reduce the risk of injury.
Thirdly, they help with your pre-exercise Mental Preparation. Dynamic warm-ups engage your mind and they can help you focus, improve coordination, and enhance neuromuscular activation. They provide a good way to listen to some music and get in the zone!
In contrast to dynamic warm-ups, static warm-ups involve holding a stretch or stationary position for a prolonged period, typically around 20-30 seconds. Static stretches target specific muscle groups and aim to improve flexibility and soothe “tight” areas. While static warm-ups might not be as effective for every type of workout, they can still offer some of the following benefits:
They increase your flexibility. Static stretches allow your joints to tolerate greater ranges of motion and therefore improve their overall flexibility. This can be advantageous for activities that require a greater range of motion, such as yoga, Pilates, or martial arts. They can be used after exercise as a good way to prevent delayed onset muscle soreness.
Choosing the Right Warm-Up The decision to opt for a dynamic or static warm-up depends on various factors, including the type of exercise, your fitness goals, and personal preferences. If we had to choose one, we mostly advocate for more of a dynamic warm up approach, since the benefits are suited to various activities, whereas static stretching is more for sports and exercise where you require greater ranges of motion.
So with that out of the way, here are a few guidelines to consider when selecting your warm-up:
1. Dynamic Warm-Ups: Best for activities involving explosive movements, sports, or high-intensity exercises. - Ideal for improving range of motion, agility, and overall performance. - Recommended before cardio-based workouts, strength training, or plyometric exercises.
2. Static Warm-Ups: Suitable for activities that require increased flexibility and muscle relaxation. - Ideal for low-intensity workouts, yoga, or activities focused on balance and control. - Can be used as a cool-down method post-workout.
Concluding thoughts: In the dynamic vs. static warm-up debate, there isn't a one-size-fits-all answer. The best approach depends on your specific workout routine, personal goals, and preferences.
Ultimately, the most effective warm-up is one that you enjoy and that adequately prepares your body for the demands of the activity you’re about to do. Listen to your body and try experimenting with different warm-up techniques over the next few weeks and see which type you like!
Ergonomic Tips and Exercises for Preventing Workplace Injuries
In this blog post, we will explore essential ergonomic tips and exercises to prevent common workplace injuries.
In today's fast-paced work environment, preventing workplace injuries is crucial for both productivity and employee well-being. By implementing ergonomic practices and incorporating targeted exercises, employers can create a safer and healthier work environment. In this blog post, we will explore essential ergonomic tips and exercises to prevent common workplace injuries.
Set Up an Ergonomic Workstation: Create an ergonomic workstation to reduce the risk of injuries:
• Choose an adjustable chair that supports the spine's natural curve and allows feet to rest flat on the floor.
• Ensure the desk height is at elbow level, allowing for a 90-degree angle at the arms.
• Position the monitor at eye level, about an arm's length away.
• Keep the keyboard and mouse at a comfortable distance, allowing for relaxed arms.
Take Regular Breaks and Stretch:
• Combat the negative effects of prolonged sitting with regular breaks and stretching:
• Perform neck stretches by gently tilting the head left and right, bringing the ear toward the shoulder.
• Roll the shoulders forward and backward in circular motions to relieve tension.
• Stretch the wrists and fingers by applying gentle pressure and performing circles and finger stretches.
Maintain Proper Posture: Maintain good posture throughout the workday to prevent back pain and strain:
• Sit up straight with relaxed shoulders aligned with the hips.
• Support the lower back with a lumbar roll or cushion. ➢ Avoid slouching or hunching forward while working.
Encourage Physical Activity: Promote physical activity outside the workplace to enhance overall health and reduce the risk of injuries:
• Encourage walking, stretching, or exercise classes during breaks or outside of work hours.
• Engaging in regular physical activity strengthens muscles, improves flexibility, and reduces the likelihood of injuries.
If you or your employees experience workplace injuries or needs professional guidance, Reload Physio is here to help. Our experienced team of physiotherapists specialises in treating and preventing workplace-related injuries. With our expertise in ergonomic assessment and personalized exercise programs, we can assist in optimizing workplace ergonomics and developing strategies to prevent injuries.
Concussions 🧠- A Physio Perspective
What is a Concussion? what are the symptoms and what can be done to help with the recovery? Physio Jemima Spike, shares some of her knowledge on the topic.
Concussion. It is in the news, we know it is bad but what is it? We know that it causes people to have a mandatory 2 weeks off sport but why?
According to the Berlin Consensus statement on concussion in 2017, they describe it as: “A traumatic brain injury induced by biomechanical forces”.
The truth about concussion is that even though it can't be seen it is a real injury. It is actually a metabolic and physiological change in the brain's chemistry. Initially after a concussion injury, the synapses in your brain fire off in this electrical storm and then have a sudden decrease in energy. The problem is when we don't give our brain the time to heal itself and return to metabolic homeostasis. This can be the cause of symptoms such as fatigue, headache and some of the others listed in the list above.
The Berlin statement reported that if any of the following are experienced after a knock to the head or enough force applied to any other area of the body a concussion can be suspected:
Symptoms: somatic (e.g. headache), cognitive (e.g., feeling like in a fog) and/or emotional symptoms (e.g. lability)
Physical signs (e.g., loss of consciousness, amnesia, neurological deficit)
Balance impairment (e.g. gait unsteadiness)
Behavioural changes (e.g. irritability)
Cognitive impairment (e.g. slowed reaction times)
Sleep/wake disturbance (e.g. somnolence, drowsiness)
Seeing your medical or healthcare professional is an important step if you suspect you or a family member might have a concussion. Often waiting until you have been symptom free for 24 hours means you are ready to progress and gradually participate in more activities. Giving your brain time to heal and a gradual return to work or sport is often recommended to get you back to your full potential.
Sometimes symptoms can linger for longer. If symptoms persist for more than 3 weeks, it can often be called PCS or Persistent Concussion Syndrome. Treatment for PCS often involves input from a multidisciplinary group. However, a Physiotherapist's role in concussion often includes:
An individualised symptom-limited aerobic exercise programme in patients with persistent post-concussive symptoms associated with autonomic instability or physical deconditioning.
A targeted physical therapy programme in patients with cervical spine or vestibular dysfunction, and
A collaborative approach including cognitive behavioural therapy to deal with any persistent mood or behavioural issues.
So, if you or someone you know isn't sure if you have a concussion and you are experiencing one of the above symptoms, chances are you have a concussion and should see a health professional with specialised training in management of concussions, so you can get back to what you love quicker!
At Reload Physio, Olivia N is experienced in the Physiotherapy Management of Concussions. Olivia can help you get back to what you love as soon as possible.
McCrory P, Meeuwisse; W, Dvorak J, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016 British Journal of Sports Medicine 2017; 51:838-847.
GLA:D - A Better Alternative for Hip and Knee Arthritis
The GLA:D Program is an evidenced based functional strengthening program for those suffering from hip and knee osteoarthritis wanting an alternative to surgery.
Osteoarthritis of the hip and knee is one of Australia’s leading causes of physical pain and functional limitations. It may start of as a niggle, and if you’re one of the fortunate ones it can stay that way. In others it can become a debilitating condition, keeping you from people and things that you love. A common perception is that a joint replacement is the end result. But what if I told you that there’s a proven alternative? Where should you go when the aches and pains start calling?
“If something hurts, it is causing damage right?” Wrong.
“I’ve been told it’s bone-on-bone… that can’t be good can it?” That’s a common misunderstanding.
“Is surgery my only hope now?” No.
One of the biggest issues facing sufferers of osteoarthritis (OA) is the confusion about what it is, and how to best manage it. There’s conflicting information everywhere, on the internet, TV shows, drug companies, well-intended health care professionals, and old wives’ tales that dominate the schooling around OA. Physiotherapists, doctors and researchers have a BIG job on their hands to help re-educate the public on the best management of OA.
Osteoarthritis is a type of arthritis that affects a joint including the bones, cartilage, ligaments and surrounding muscles. It is often described as a wear and tear issue but is better described as a joint that is ‘working overtime’ trying to repair itself compared to others.
The GLA:D Research (Good Life with Osteoarthritis in Denmark) found that medication, rest, massage, and surgery were NOT the first line treatment methods for hip and knee OA.
Mind blown.
The best results shown to treat hip and knee arthritis as a first line defence goes like this:
Functional strengthening – targeting key muscle groups at the right dosage for every person.
Education – about arthritis, it’s symptoms and best management (you’re currently reading a big chunk of it, winning).
Weight loss – even losing a little can make a big difference. We are here to support you.
What do you mean by functional strengthening?
No, it does not mean getting bigger biceps, or tree trunks for thighs.
Functional strengthening targets essential muscles in a way that mimics daily activities or tasks. For example, getting up off a chair, and walking up and down stairs. Even doing some time on a stationary bike can be helpful to build cardiovascular fitness, and build strength that benefit arthritic hips and knees.
It helps to improve your ability to control movements to lead a healthy active life. Often, due to pain or stiffness moving well can be lost, making symptoms worse than what they need to be. The GLA:D program aims to help restore this movement!
The GLA:D Program Results speak for themselves
There are over 50 randomised controlled trials (a very good source of evidence) that have been proven that exercise is effective for arthritis of the hip and knee. Unfortunately, there as inconsistency with how the researchers described the actual exercises, and what the long-term benefits were. That’s when the GLA:D program was started to solve these mysteries. They came up with standardised exercises that were delivered by physiotherapists with specialised training, and measured in a consistent way!
They found that best results were obtained with an exercise program that lasts a minimum of six weeks. Each exercise session is an hour long and performed twice per week. Sessions need to include the key exercises to improve strength, movement quality and confidence in your hip or knee. Education is the cherry on top and can’t be left out.
As time goes on the evidence only gets stronger, as more and more physiotherapists and researchers expand the program across the globe. They are now using the data to help inform policy makers and to educate health professionals and the wider community. Wives’ tales will be no more.
The proof is in the pudding. With the data of 18,000 + patients, the results speak for themselves.
A year after starting the GLA:D program OA sufferers reported:
A 32% reduction in pain (that’s pretty big for a chronic injury)
Decreased use of medication
Less sick leave was taken
They got stronger
High satisfaction scores
Reload Physio has been performing the GLA:D program for nearly two years and our patients have had some pretty amazing outcomes. Some have postponed their up-coming surgeries, others dusting off their well-loved hiking boots, while some reduced the need to be up throughout the night due to pain.
We have physios trained in the GLA:D program who are already implementing the world’s best functional arthritis management. If you’d like to join the growing team of Brunswick locals who’ve already found an alternative to medication and surgery, give us a call to arrange a session. Or alternatively, get in touch to find out more information.
In the meantime, have a listen to one of GLA:D’s founders, Prof Ewa Roos: https://www.youtube.com/watch?v=B2XMszQP_pY
ACL Injuries
Eran explains the basics of ACL rehabilitation and the need for sport-specific training before returning to the field.
With the sporting season currently on hold, it is the perfect time to prepare your body for the impeding demands of a full season and rehabilitate any injuries that you might have. It is the time to work hard at your strength training, mobility work and motor control deficiencies. Today I will focus on the anterior cruciate ligament of the knee, otherwise known as the ACL. As a retired athlete I have torn my ACL too and I have learnt first hand that a full recovery does not involve any shortcuts. Marcus and I attended a conference on ACL rehabilitation by Mick Hughes in February this year to make sure we are up to date with the latest research and evidence based practice.
What is the ACL and how does it get injured?
The ACL is a ligament in the knee that resists excessive movement of your shin and thigh bone on top of one another, namely anterior translation and rotation. It provides a significant amount of stability and attaches from the anterior portion of your tibia (shin bone) to the posterior portion of your femur (thigh bone).
The ACL is most likely to sustain an injury from a non-contact movement. For example, landing from a jump in netball, or cutting and side stepping in a footy match.
We know that female soccer (football) has the highest rate of ACL injury, followed closely by basketbal and AFL. The reason these sports have higher risk relates to the movements required by each sport. For example, in both AFL and soccer there are a lot of hard cutting and change of direction movements. In AFL and basketball a lot of jumping and landing that athletes need to train for to condition their bodies to tolerate and become efficient at the movements.
Following on from the stats above, you can see that being female does increase your chance of sustaining an ACL injury, sorry ladies. This is because females physiologically have a wider pelvis (bigger angle towards the knee), your hormones (oestrogen) can influence how ‘loose’ the ACL is; and the size of the bone area where the ACL attaches into is smaller.
What does a typical ACL injury look like?
Basic anatomy of the knee
Typically, a “pop”, “crack” or “snap” is heard at the time of injury. Secondly, a sharp, sudden pain is felt with the athlete grabbing at their knee. Thankfully, the pain does not usually last long but the knee feels unstable followed by immediate balloon-like swelling within the first 10-20 minutes which tends to worsen over the following 24 hours.
* The most suspicous sign for coaches or side-line physiotherapists to look out for is if the player immediately grabs their knee.
In the short term walking is difficult and assistance in the form of crutches, a stick or someone to lean on, might be required. However, this is not always the case! Numerous players who’ve suffered an ACL injury only complained of a swollen knee. So it is always worth getting a full assessment done if your leg does not feel ‘quite right’, feels unstable or weak as there are different degrees of ligament injury.
What to expect during your physiotherapy assessment
Your physiotherapist will perform a number of clinical tests to reach a definitive diagnosis and establish an individualised treatment plan. He or she will test the integrity of all the ligaments, menisci and cartilage in your knee, assess any swelling inside your knee capsule (intracapsular swelling), look at your strength, stability and perform a few functional tests. If an ACL injury is suspected you will likely be referred for an MRI to confirm the diagnosis and assess the severity of your injury, and to see if any other structures in your knee have also been affected.
In the meantime, you will receive support in the form of bracing, taping and compression, crutches (if needed), reassurance and a few home exercises to improve your rehabilitation outcome.
Conservative management vs surgery
Not all ACL injuries are the same, therefore some have fantastic outcomes with rehabilitation, while others would benefit from early surgical intervention. The answer will be based on each individual’s injury, the extent of damage, initial management, level of sport etc.
How long until I can return to sport?
The general rule of thumb is to wait a minimum of nine months before returning to sport, provided you have done a full nine months worth of rehab to prepare you for it. The rehabilitation period differs for each individual and should be guided by a trained and qualified physiotherapist.
Your physiotherapist should put you through your paces with a variety of tests to ensure your body is ready for the demands of your sport. Testing the strength, stability, mobility, motor control and skills (co-ordination, reaction times, jumping, landing etc.) to pick up any deficiencies if present. In my own journey, I waited ten months before I went back to gridiron after being cleared by my physio’s specific and brutal discharge criteria.
Just waiting nine months and going right into a game isn’t going to cut it and will put you at risk of re-injury. This is because that for every one month you return to sport before the recommended nine your chance of re-injury is 51%!! If that doesn’t scare you into doing your exercises then I don’t know what will.
If you have injured your knee and aren’t sure what the next steps are, contact us at Reload Physio. We can guide you through a thorough individualised rehabilitation program to get you back to sport safely, at the highest level.
Can you be proactive to prevent an ACL injury?
The short answer is yes, you can.
Lets consider what movements are known to cause an ACL injury: non-contact landing and cutting. You are able to train your body to get used to these movements over a period of time to prepare for the unpredictable nature of sport.
There are many prevention programs out there that have been validated to reduce the risk of ACL injury, and are used by professional, and competitive athletes around the world. One of the most well known programs is the FIFA 11+ for soccer, which runs through a variety of different exercises that are performed during pre-season and in-season conditioning. It is still being validated for other sporting codes, such as netball.
If you think you or your team could benefit from a program such as FIFA 11+ please contact us at Reload Physio for more information.
Happy Monday everyone.
Pregnancy related Hand and Wrist Injuries
Physio Carla Bywater delves into wrist and hand injuries during pregnancy and post-partum.
In-Clinic or Telehealth consultations are very effective and available to help you manage these conditions.
Pregnancy is such an exciting time filled with anticipation and wonder for what’s to come. I always have so much admiration for the female body, transforming, creating, shifting and nourishing to create new life. As part of a new blog series covering some of these changes and challenges women experience, we will look at carpal tunnel and ‘baby wrist’ today. I personally experienced a very painful wrist on my left from carrying and holding my newborn daughter in “all the positions” to feed, rock to sleep, to hold and to cuddle. It started off as a mild discomfort but before long I could hardly use my left hand!
Below is some information if your wrists are also giving you grief during pregnancy or beyond, and what you can do to manage it.
Carpal tunnel syndrome
WHAT IS IT?
Median nerve related neuropathy affecting the first three and a half fingers. It results in pain, pins and needles, numbness, a weaker grip and if severe can result in muscle bulk loss.
The carpal tunnel symptoms experienced during pregnancy is largely due to an increase in fluid retention throughout a woman’s arms, compressing the median nerve.
Carpal tunnel symptoms after pregnancy e.g. fourth trimester, is most commonly a result of wrist positioning and prolonged flexion while holding, breast feeding and caring for a newborn babe.
Lets tackle carpal tunnel during pregnancy first…
Pregnancy-related Carpal Tunnel
Normally you will experience symptoms in both arms, and you’re likely to notice swelling (peripheral oedema). Do you notice that your rings now fit uncomfortably on your fingers, or you have to remove them completely?
Looking at a ‘normal day’ your symptoms tend to be worse in the morning and evening, but eases during the middle of the day. Night time can be pain with increased sensations of pins and needles or pain, especially if you curl your wrists into a flexed position while you sleep.
It often gets worse as your pregnancy progresses
Clinical tests performed by your physiotherapist will be able to confirm your diagnosis of carpal tunnel.
Things we can do to help:
Wrist orthoses and advice. Based on a study in 2006 with 30 women, 83% had a reduction in symptoms after only three weeks. Winning.
Ways to manage the swelling such as soft tissue work, compression and positioning might be helpful on an individual basis.
The good news? Carpal tunnel syndrome after pregnancy tends to go away relatively quickly. A small number of women are likely to suffer in the long run based on how severe their symptoms were during pregnancy, how soon it started and if they scored high on the Endenburg Depression Scales after giving birth.
Carpal Tunnel in the Fourth Trimester
Here symptoms are associated with prolonged wrist postures whilst breastfeeding. Often wrist flexion postures are needed for hours on end and as a result, symptoms can start within two weeks of breastfeeding.
The symptoms lasts around five to six months therefore, it is important to get an assessment and treatment as soon as possible. Advice and a few home exercises can go a long way to help with spinal mobility, neural mobility, posture, pain and other symptoms.
If symptoms become more serious with associated weakness and numbness it increases the risk of the mother dropping her baby... we do not want that, so please get in touch sooner rather than later.
“Baby Wrist” aka De Quervains
WHAT IS IT?
Baby Wrist is also known as De Quervains Tenosynovitis.
It affects women (and men) post-natally due to repetitive lifting of your baby.
‘Baby wrist’ is caused by an injury to two of the tendons that attach into the thumb. As a result they struggle to slide and glide during normal range of movement.
Symptoms include pain, swelling and tenderness around the base of the thumb down to the wrist.
What can we do to help?
Good news is that 75-95% of mild cases can be treated conservatively by your physiotherapist! Lifting advice, ice massage, splinting and taping have been proven to be very effective.
If the symptoms do not subside with the above treatment, a corticosteroid injection may be considered.
TFCC - Triangular Fibrocartilage Complex Injury
In my case, my wrist pain was on the side of my pinky, just above my ‘wrist bone’ where my TFCC is located. It is less commonly injured during pregnancy and post-natally in comparison to others, however, if it does occur it is helpful to know a bit more about it.
WHAT IS IT?
Your TFCC is a small cartilage disc located between the end of your ulna, and some of the smaller bones within your wrist (carpal bones). The TFCC helps to stabilise your wrist, and allows your wrist to move like it should. When injured the area is painful and often swollen, it can also ‘click’ or feel ‘stuck’. For example, in my case, it was very painful to rotate my hand, wrist or forearm, any weight bearing positions was also a big no for me.
Once I realised that something had to give, I took my own advice (and that of my husband!) and changed how I handled my daughter, I iced, massaged, tape and mobilised the area.
Furthermore, due to breastfeeding 24/7, I became a bit ‘hunched’ with reduced movement through my upper back. Reduced thoracic spine mobility directly affects the biomechanics of the shoulder girdle and arm, further increasing the load through my wrist.
See below for three stretches that I used to improve my upper back mobility during pregnancy and in the fourth trimester.
You’re welcome.
Exercises to improve your upper back mobility:
Whether you suffer from carpal tunnel irritation, or de quervains - these three exercises will allow your thoracic spine to move more freely, reducing the load through your arm and wrist.
Thread the Needle
Take three breaths at the end of the movement. Repeat x 5 each side. Thank me later.
Thoracic Extension
Hold for 30-60 seconds. Move the roller down your back to work on different spinal segments. It does get easier trust me.
Modified Childs-pose Stretch
This one targets your Lats. Hold for 60 seconds each side. Breathe deeply into your lower ribcage.
If you are suffering from any hand or wrist pain or stiffness while pregnant or while keeping a little human alive, please reach out for help!
We have physiotherapists who have an interest in women’s health and can help you now. Whether you are local to our practice, or distant to us, we can help with both in-rooms or Telehealth consultations
Book youR In Rooms or Telehealth consultation now.
De-mystifying lower back pain
Physio Stephen Vong outlines many of the myths and beliefs regarding lower back pain, including disc bulges, need for MRI scans, chronic back pain and more.
We have been getting a lot of Telehealth consultations this week from clients complaining about lower back pain! Whether or not it was due to the increased stress associated with isolation, social distancing, working at a less-than-ideal home office, or lifting their child out of their car seat that caused your back pain! So, I thought I can demystify lower back pain for you, so that you know how you can self-manage at home, or when to seek professional guidance from your physiotherapist.
What is low back pain?
Low back pain is an umbrella term!
It’s a symptom rather than a disease and can result from several different known or unknown abnormalities or injury. Some discomfort can come on suddenly while you were doing something, or some build up gradually over time.
Lower back pain is commonly accompanied by pain in one or both legs. Some people with low back pain also have associated altered sensations in their legs, such as tingling. Low back pain is usually non-specific; this means that the pain cannot be attributed to just one cause but rather a combination of different factors (joint stiffness, age-related bony changes, nerve compression) – this accounts for 90% of people with low back pain.
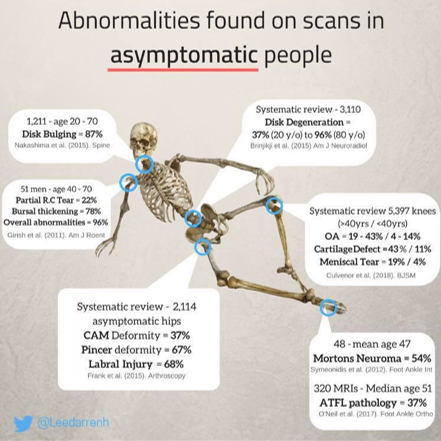
Myth 1: I need a scan for my lower back
Many sufferers of low back pain receive routine spinal imaging (CT, MRI) despite evidence-based recommendations that ONLY call for imaging in people with worsening symptoms or neurological deficits. For example, those who lose feeling or strength in their legs, or lose control of their bowel or bladder.
We often hear clients say: “I did an MRI/X-Ray recently and they found that I have degeneration of my spinal segments, or “I have a bulging disc” and it leads to the assumption that something’s damaged, or that something is “out of place”. This tends to cause a ripple effect, where people believe they need a “fix” a problem that has been identified on scans.
In fact, many high-level studies have shown that there is a poor correlation between imaging results and symptoms. AKA what shows up in the scan might not be the cause of your pain AT ALL. Or, you can be in significant pain, but your spine looks ‘normal’. Where does that leave you?
Although there are specific pathological causes (disc degeneration & spondylolisthesis) associated with an increased risk of lower back pain, no evidence exists that imaging improves patient outcomes. On the contrary, scans may lead to poorer health outcomes, greater disability and work absence due to ‘pathologising’ the problem! In reality imaging should be used to rule out serious conditions only, rather than “fishing” for a diagnosis.
Myth 2: Pain means I’m damaging something!
Pain is multi-factorial! Factors such as circumstances, previous pain experiences and coping styles all affect the way we perceive pain.
Pain is a protector – by making unpleasant feelings, your brain changes your behaviour in order to “avoid” injury to allow tissue to heal. Usually, a stimulus – the pain perception – is relayed to your brain, which then regulates the level of your response – the pain reaction. During injury however, this process is enhanced. This may cause a higher-than-usual pain reaction to the same amount of pain perception. Therefore people with similar back issues can experience pain very differently – it not just a matter of “high pain threshold”!
Myth 3: “Slipped disc”
The term “slipped disc” often causes many to visualise a portion of the spine dislocating in the body. In fact, the medical term “slipped” isn’t remotely accurate to what happens. Each disc has two portions: the harder outer ring, and a gelatinous inner portion. When a disc “slips” or herniates, the gelatinous inner portion pushes into the tougher outer ring, causing pain and discomfort.
Sometimes, it may rub into your spinal nerves and cause inflammation of the nerve, leading to numbness and pain along the nerve. However, because the spinal column is a small space with an intricate network of blood and nerves, an inflamed disc can place extra pressure on the surrounding structures such as soft tissues, muscles, nerves & ligaments without trying too hard.
Depending on the degree of herniation, it may dictate the symptoms experienced, and time taken to recover. Symptoms are usually short-lived as the localised response settles down, and the body becomes accustomed with the shift of the disc. Thank goodness! Studies have shown that discs are reabsorbed into the body in six to eight months, but symptoms can be as short as two days!
Myth 4: I need surgery!
Renowned physiotherapist Peter O’Sullivan said in a recent interview that:
“For someone without private health insurance, it would be cheaper for someone to go through the public system and have spinal surgery, than to see a physiotherapist for a course of education and progressive exercise”.
That in itself sounds ridiculous! Think about it…
The primary rationale for surgery is that it will relieve root irritation or compression, and in turn, lead to less pain. However, several studies comparing surgery & conservative management (physiotherapy) have found that:
• Benefits of conservative management is equal to surgical intervention in terms of pain, symptoms and quality of life.
• No reduction in sciatica (nerve pain down the back of your leg) or improved quality of life between the two groups.
• In disc-herniation surgical studies versus conservative management, pain is relieved earlier in surgical groups, but were no different at 12 weeks later between the groups.
Emerging evidence suggesting a conservative approach to management of lower back pain as the primary course of treatment because patients tend to improve with or without surgery. This does not say that surgery is not at all required. Patients who continue to have debilitating or progressive neurological deficits despite initial physiotherapy management may need a referral to a surgeon.
Myth 5: Now that I have back pain, I’ll have it forever
If you have acute low back pain you need to be aware that your pain levels will take time to decrease when engaging in your individualised exercises and is not immediate. Recovery and pain actually take longer with complete rest and inactivity. So, keep moving people!
You can usually recover from back pain within a few weeks and continue to improve over a few months. Recurrences of low back pain are also common, with evidence showing that 33% of people will have a recurrence within a year after you recovered. Unfortunately, 10-15% develop chronic low back pain, with 78% suffering from relapses. However, chronic low back pain is often seen to be attributed to factors that may be work-related, related to personal/family issues and/or psychological health.
While it is tempting to refrain from all physical activity while you’re experiencing pain or discomfort from your back, this can lead to higher levels of pain, greater disability and poorer recovery. Furthermore, movement prevents maladaptive movements (such as avoidance behaviours) which may be detrimental in the long term. Instead, try to remain as active as possible with low impact activities such as walking or gentle stretching.
The Reload Team: Our role as physiotherapists is simple:
• Relieve the pain. Manual therapy in the acute & subacute phases allows us to restore mobility in stiffer joints and reduce muscular tension. It also opens a window of opportunity to allow for more movement. Manual handling will be limited due to the current pandemic, however self release work at home is invaluable and we will give you clear instructions on how to do so safely.
• Regain the movement. Exercise prescription and guidance to ensure you’re performing the movements correctly and progressing them appropriately. Immobility/reduced movement often leads to poorer outcomes, so it is imperative that we normalise movement behaviours as soon as possible!
• Reload for resilience! Become stronger than when you started!
At Reload Physio we recognise that there is no “one size fits all” exercise protocol, but we aim to create one that is both individualised & achievable for you. Having the appropriate equipment for strength & conditioning, and movement control allows us to tailor a program together.
If you would like more information, please get in touch by phoning our lovely reception staff, or booking yourself in for a Telehealth consultation.
We are currently offering free 15 minute phone consultations if you have any questions instead of our usual injury screening appointments.
Osteoporosis, Osteopenia - Onero Classes for your bone health
If you’re already a patient at Reload Physio you may have noticed ONERO on the class timetable. Today we further our discussion around bone health, this time focusing on an evidenced based exercise program to help increase bone density and strength. Due to current social distancing measures we discuss how we can now offer modified ‘bone health’ classes for you to do from the comfort of your own home!
Have you heard of osteoporosis or osteopenia?
Osteoporosis is common condition affecting over 1 million Aussies. It is a disease that causes our bones to become weak and brittle which results in a higher chance of a fracture (break) when we trip, stumble or topple over. Bone is a living tissue that is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone doesn't keep up with the loss of old bone.
The primary method to diagnose osteoporosis is the use of a bone density scan, which is ordered by your general practitioner (GP). The test can not only tell us if you have osteoporosis or normal bone density, but can also let us know if you are on the road to developing osteoporosis (AKA osteopenia). Osteopenia is when our bones are classified as weaker (or less dense) than normal, but not quite as weak as those with osteoporosis.
“It was after diagnosis of osteoporosis that my smart thinking GP flagged the existence of the Onero programme in 2019. I had never heard of Onero but was determined to do all I could to stay upright, to stay strong and do all I could to manage the symptoms of Osteoporosis in my spine - Ruth”
There are many risk factors that make us more likely to develop osteoporosis. Some we have control over, others we do not. Lets cover the ones we do NOT have control over first:
Ladies, we are out of luck here - we are at higher risk. This is due to the reduction in oestrogen levels as we age, specifically during menopause.
If you are older than 50.
Having a family history of osteoporosis.
Certain medications (for breast cancer, prostate cancer, epilepsy and some anti-depressants).
Medical conditions, including but not limited to, thyroid disorders, coeliac disease, inflammatory bowel disease, rheumatoid arthritis, chronic liver or kidney disease.
On a positive note, things that you do HAVE control over, and can change, include:
Low levels of physical activity
Smoking
Excessive alcohol intake
Your weight (thin build or excessive weight).
Low levels of calcium or vitamin D
I know that new year resolutions have probably been and gone, but there’s nothing like another motivating factor to get your health in check again! Especially with more time on your hands during the current COVID-19 saga.
Therefore, it is important that if you suspect that you have osteoporosis to see your GP as soon as possible. The sooner you know, the sooner we can treat the condition and start to improve your bone health together. Interventions may include improving your nutrition; taking vitamin D and calcium supplements (and don’t forget some time in the sun!), specific medications and a supervised exercise program. We can refer you to a fantastic dietitian, but our specialty is to get you moving!
Onero ™is an exercise class that is designed for clients who are catergorised as being at a higher risk of developing osteoporosis, the program is designed to reduce their chances of osteoporotic fracture by stimulating bone growth and preventing falls.
But hold on… is there any evidence to back this up?
Research demonstrates that only certain types of exercise can improve bone health. All of which are included in the Onero ™ classes! Evidence shows that the specific exercises twice a week is enough to stimulate bone growth, improve muscle strength and help to reduce the risk of falls. In fact, the original research that underpins Onero™ included only one hour of exercise a week!
In order for the program to be safe and effective for patients with OP it must be supervised by a physiotherapist who is trained and licensed in teaching the Onero™ program. At Reload Physio we have four Onero™ licenced clinicians – Marcus, Adrian, Jess and Eran.
“After an initial assessment, Onero provides a programme of gradually increasing resistance, weight bearing exercises, within in a super friendly small group environment, to build strength and physical resilience - Ruth”
Think you have frail bones and unsure if Onero™ is for you?
If you have been diagnosed with osteopenia or osteoporosis you are eligible to give it a go! But if you have FOMO you can still get involved, even if you have normal bone density. The class will also help to maintain and improve your bone health. How good?!
“I feel the difference Onero has made to me: sure I still have Osteoporosis and I must manage that lifelong, but part of that ongoing management includes continuing Onero for as long as I can get out of my front door. the investment in your body is well worth it. We need to keep out bodies strong, give Onero a go! - Ruth”
Can I still take part if I have a few other health concerns?
Absolutely! Onero™ licenced physiotherapists are trained to safely adapt and deliver the program to those with other co-morbidities so that you can safely participate with less risk of injury or fear of exacerbating existing conditions.
So there are no excuses not to work out for 40 minutes and improve your bone health while doing so.
Want to know more?
Even with current climate we can keep you fit and healthy via our Telehealth consultations and provide you with a tailored exercise program.
We are also live streaming modified classes online to keep you healthy - they are called Bone & Balance and you do them from the comfort of your own home. Minimal equipment is required. Please contact reception for more information.
Alternatively, you can book in to talk to one of our clinicians during a Telehealth consultation to ask any questions that you may have about osteoporosis. To book click here.
For some light reading:
Beck BR and Weis LJ: Translating high intensity loading for osteoporosis to the real world: Two year observations from The Bone Clinic. Research to Practice Annual Scientific Meeting of Exercise and Sports Science Australia, Brisbane, Australia, 27-29 March 2018 (Winner: Practitioner Award)
Osteoporosis Australia. (2014). FAQ. Retrieved from https://www.osteoporosis.org.au/faq
Physiotherapy for Women through their life stages
A fantastic outline about the importance of Women’s Health from Physio Anneka Mathias. From Puberty, through the Pregnancy and parenting years then on to Menopause, the guidance of a Physio with special interests and training in Women’s Health can help you along the way. From Pelvic Pain, to your ‘waterworks’ and other physical challenges Physios Anneka, Carla and Grace can help you through- Telehealth services available too.
Well where do I start?! The miracle that women thrive throughout our life stages still astounds me. Puberty, adolescence, the childbearing years and menopause all include major hormonal and structural shifts and adaptations. Not to mention the usual process of aging, work and daily tasks, family life, relationships, exercise and sport. Wow. Might I hit a few nerves by saying that our male counterparts have a slightly ‘easier’ deal?
To cover it all in one go will be lengthy, so let us focus on the childbearing years and see how a physiotherapist can help you, or loved ones, through the physical changes and new demands that are placed on the female body.
Women have given birth since day dot. Beautiful changes occur in your body to grow and nurture another little human inside you. Your pelvis widens, your rib-cage expands, organs shift to make room for your ‘mini-me’ over nine or so months. Feeling flutters of movement as the weeks pass make it more and more real, your life as you know it is changing. Unfortunately, all of these beautiful changes can also result in less ‘glamorous’ aspects of pregnancy. Fatigue, wakefulness at night, aches and pains, nausea, cravings, body temperature changes and more frequent trips to the toilet are all considered ‘normal’.
Then there is giving birth, or the birthing process, that looms at first far in the distance, and then it is upon you. Birthing and antenatal classes, books and advice from your midwife has prepared you up till now. Occasionally, it does not go to plan, often it does. Nevertheless, the post-natal period (the fourth trimester) is not talked about freely, at a time where you need support the most. Often, we hear women say, “I didn’t know there are physiotherapists who treat this” or “I thought that this was normal”. A physiotherapist with an interest in women’s health, or a titled women’s health physiotherapist can help.
In October 2019 the APA (Australian Physiotherapy Association) released a statement calling for ‘women’s health physiotherapists to be included in the care teams for all pregnant women in Australia to reduce the risk of complications and to improve outcomes for women and their babies’.
Currently in Australia, access to obstetric physiotherapy care is available to women in some areas but not in others, meaning thousands of women every year are missing out on getting individualised care to support them during pregnancy and their recovery after birth. We are here to change and challenge that norm. All women deserve to be cared for during this time.
BUBS-IN care
During pregnancy, we can give you advice on how to exercise and modify daily activities as your body changes, as well as help you prepare your body for labour. We are available to treat any aches or pains including wrist pain, pelvic girdle pain (PGP) and back pain.
Pain around your hips, back and pelvis?
PGP is common and normal during pregnancy. Most women will start to experience it between 14 and 30 weeks, but it could sneak up on you earlier or later as your body adapts to growing a baby. Symptoms may include pain with walking or turning over in bed, at the front or back of your pelvis, sometimes radiating down your thigh. You may find yourself unable to sit or stand for long periods of time. Physiotherapy treatment is used to slow the progression of PGP during your pregnancy, and make you more comfortable leading up to birth.
Getting tingly hands and fingers?
Many women experience carpal tunnel syndrome or similar symptoms during pregnancy. The carpal tunnel is a small passage in the wrist where nerves and tendons pass from your arm into your hand and fingers. The hormonal changes that occur during pregnancy cause you to retain fluid and they softens the ligament which forms the roof of the tunnel. When this happens, the nerve that runs through the tunnel can become compressed resulting in pins and needles, numbness and stiff painful hands. The good news is that there are many ways physiotherapy can help, and most women are able to significantly decrease their symptoms.
Keen to exercise during pregnancy but need a bit of motivation?
We offer great BUBS-IN exercise classes to keep you moving. We are now offering them online via a live stream as an option during this time of social isolation, as exercise during pregnancy has been proven to improve health outcomes for both yourself and your baby.
BUBS-OUT care
After you give birth, all the love and attention are often focused and diverted on your gorgeous little human(s). However, your body has just gone through major trauma and/or surgery, alongside sleep deprivation and exhaustion. YOU need time to heal and recover to be the best mumma for your bub in the long run. Physiotherapy can help with a wide range of conditions post birth including incontinence, pelvic girdle pain, mastitis symptoms, abdominal muscle separation, scar tissue management and symptoms of prolapse.
Prolapse, what?!
Pelvic organ Prolapse (POP) is the downward displacement of pelvic organs (bladder, bowel or uterus) resulting in movements towards or through the vaginal or anus. According to the APA - In Australia, it is currently estimated that 50 per cent of women who have had more than one child have some degree of pelvic organ prolapse.
Prolapse is normal but it comes with a range of symptoms such as heaviness, dragging, low back ache, interrupted urine flow and leakage. There are different degrees and types of prolapse therefore, if this sounds familiar, or you have been told by a health professional that you might have a prolapse, or you simply would like to have your pelvis assessed, get in touch with a women’s physiotherapist.
Leaking?
Leaking can be embarrassing, socially isolating, reduce your physical activity, and it can negatively impact on your sex life. No wonder it is linked to higher rates of depression.
We recommend that you get a post-partum assessment around the six-week mark. It will give you a great opportunity to ask questions, look after YOU, and allow us to do so. Your consultation will be professional, private and in a safe environment. Your therapist will also talk about your goals and expectations for recovery, what you would like to get back to doing (returning to hobbies, exercise or work) and provide you with education and guidance you need to do so safely.
You can even bring your wee one in with you too, we LOVE babies! Futhermore, Telehealth consultations are now available so you can access great education and care from home! Voila! Because lets be honest, if you make it out of the house you’re winning. So no more excuses, all you need is a stable internet connection and you’re good to go!
It is vital to have a formal and thorough assessment and provide you with a series of options for your own individualised treatment, or simply reassure you with where you are at. BUT please be patient and kind to yourself, as it is going to be a gradual process to get you to where you want to be.
If you would like further information, please do not hesitate to talk to one of the physiotherapists here at Reload Physio or book in for a consultation. Grace, Anneka and Carla all have a passion for and an interest in women’s health and well-being.
COVID-19- What we are doing, how you can help at Reload Physio
An update by Owner Marcus on everything that is being done by Reload Physio during the Coronavirus outbreak. The practice is open, we are closely following all of the recommendations to minimise the risk of transmission. We have expectations of all of our clients attending the practice and we we have our own ‘Reload COVID-19 Stimulus Package’ specials.
I would love to say it’s ‘Business as Usual’ at Reload Physio, but it is ‘Business, same but Cleaner than usual… and quieter!’
Well these are unprecedented time with this virus sweeping the globe. This blog is not going to educate you about the virus or the importance of good hygiene, how to sneeze and social distancing etc etc, that information can be found on almost every other website… I would like to inform you of everything that we are doing to minimise the risk of infection in our practice, what we ask of you, and the real effects that this is having on all small businesses across the land.
Business as usual
At Reload Physio we have always had a clean and hygienic practice, but we have dialled up our hygiene practices by a multitude of about 10!
So here goes…
We are asking every clients to wash their hands with Alco wash on entry and exit of our practice (we even have instructions about how to wash your hands effectively)
We are doing the same before and after every client… not sure how long the hand wash supplies will last but we will be sticking to this as long as we can.
We are cleaning all communal equipment - phones, keyboards, chairs, Eftpos terminals, door handles and everything else you can think of regularly.
All gym equipment is being wiped down regularly. Every class attendee is being given Alco wipes to wash their equipment at the end of each class.
All clients are requested to bring their own drink bottle, sweat towel, and grip socks to class - we have significantly discounted grip socks - 40% off if you forget or don’t have any!
We have removed the bed sheets from all treatment tables - so we can clean the beds after each and every client.
We have removed all waiting room cushions and cushions on the ‘client chairs’ in the treatment rooms - hard surfaces are easy to wipe down, soft are not so easy.
We are trying to encourage everyone to pay by card… how many germs are on cash? You can enter or tap your own card too!
We have multiple “cleaning stations” throughout the practice.
We have separated our Pilates equipment further - social distancing.
We are reducing the maximum amount of participants in our classes to also allow greater distancing.
So what else are we doing?
Telehealth consultations are going live.
What is telehealth? Let's be real, it is a glorified word for a ‘Skype call’ , It is an opportunity for someone who cannot attend the practice to still pick our brains for info, we can offer a comprehensive questioning session, make a preliminary diagnosis (without doing any hands-on testing we are a little limited), we can then provide exercises, look at your technique of those exercises, and prescribe more progressions or variations for the next step of your progression. We do these Telehealth consults through our Physitrack software where we can share the exercises and videos too, all encrypted and all linked to your clinical file. (so not exactly just a skype call- somewhat better!).
But you can’t massage me so it wouldn’t be worth it! This is a challenge we face daily- many clients put most value on the 'hands-on’ treatment that we provide, and the reality is that the most valuable part of Physio is the advice, exercise and guidance that we share with you. In most occasions, injuries heal themselves if we give them the right environment, stimulus, restrictions and also progressions for mother nature to do her thing!
How do you book? Call the practice or book online though the button below. If you require a Telehealth consultation for something we havent seen before, then book an Initial Telehealth Consultation. If we have seen you before for this problem, either in the practice or a previous Telehealth consultation, then a shorter Telehealth Review Consultation is adequate.
What can you do for us?
Most importantly, if you’re sick, contact us and let us know so we can reschedule you for a few days (or 14 days) later.
Don’t arrive too early for your appointment- a crowded waiting area is not great at this time. Wait in your car if needed.
Wash your hands when you arrive.
Don’t cancel your appointment if you are well- we are still here for you
Tell other people that we are still here... and Awesome.
Book multiple appointments or classes ahead.
If your gym is closed, talk to us about whether our services and facilities could be a temporary alternative.
If you are in Isolation, or we all go into isolation, jump back on the Reload bandwagon as soon as you can afterwards.
Don’t hesitate to contact us on hello@reload.physio if you have any questions or need any support throughout this tough period. Attention it to Marcus if required.
We are also offering some great service packages… We hope you can see the humour in the Name…
The Reload Physio COVID19 Stimulus Packages!
Physio Massage
5x Physio Massage @ 15% off
10x Physio Massage @20% off
Physio Consultations
5x Std Consults @10% off (incl 1x Free Telehealth Consult if required)
10x Std Consults @ 20% off (incl 3x Free Telehealth Consults if required)
5x Extended Consults @ 15% off (incl 2x Free Telehealth Consults if required)
20x class pack (any class) @25% off
20x any service @ 25% off
Vouchers for the future!
Vouchers - all 20% off - BUT Valid from May 2020-May 2021 (NOT valid for the next 6 weeks)
Self Treatment Stock Packages (while stocks last)
Self Relief Package 30% off
Spikey Ball or Myofascial ball + Stick On Heat Patch x3 + Tube of Fisiocrem + Short Foam roller or BakBalls
Self Rehab Package 30% off
1x Loopband + 2x Theraband or Theratube length (different resistances) + Pilates Ball + Pilates Socks
Yes, big discounts, but this stimulus is for both your health and our cashflow for the weeks and months ahead- you win-we win!!
Why are we doing these packages?
Anyone who has any accounting or business knowledge understands that the benefit of our clients buying these packages is the positive cashflow for our business. We are not shying away from the facts that we are quite likely to have to close our practice for a period of time, and upon return, there is quite likely to be an economy like we have not seen in my lifetime. Reload Physio is a small business that employs 14 people, who all rely on the income from this practice, from our clients- you, to meet their own financial obligations. Some staff have kids, some have mortgages, all have financial obligations of some sort and without income coming into the practice, we are sitting on a very shaky ground. I have full confidence that Reload Physio will get through this because we have a great team who are committed to work together, we have a great community that supports us as we support them. Community is one of our Core Values- ‘We will make our Community Better’.
In 16 years of owning the practice, we had never closed our practice for more than a long weekend or public holiday period etc, until January 2020 when we very nervously closed for 7 working days for our amazing renovation! Now 6 weeks later couldn’t be a worse time to have to do this again but sometimes life throws you a curveball (or a cannon in this case!!). Paying staff without generating income is tough, (my biggest understatement of this decade so far!!) so having to close for a longer period will even be more challenging. Any assistance from our community to assist with this cashflow over the coming weeks or months may help pay for nappies or mortgage or loaf of bread.
We welcome your ideas about how we can assist our community even more during this period, either remotely or in clinic or face to face while still possible.
He hope to see you in the practice soon, stay hygienic, stay healthy and look after those at high risk.
Regards
Marcus, Melissa and the Reload Team x
UPDATE:
Coburg Leisure Centre is now closed until the end of March (at least), so bookings cannot be made for Coburg until we have confirmation that the facility is re-opening.
RELOADing your Running- Load Management for Runners
Get a deeper understanding of how to manage your running training loads is the key to staying injury free and to help you achieve your running goals. Our Physio Grace talks through the importance of Load management and a few ways to safely manage your training.
RELOADing YOUR RUNNING
Following on from our previous two blog topics that covered energy deficiency in sport (RED-S) and bone stress injuries where both touched on managing your load as you train. Today we would like to delve deeper into load management, with a focus on running (since we love it so much!). It should give you an idea how to progress yourself safely and effectively, whilst not foregoing your performance targets in your weekly Park Run!
Load management in sport is both a science and an art. It can be thought of as the delicate balance between training and competition, and rest and recovery. It is the difference between a well beaten dollop of cream and clumpy cream but-not-quite-cheese result.
Correct load management will allow you to meet your fitness and performance goals while ensuring that you do not sustain an injury or burn-out. It will empower you to return to running safely after some time off, or to increase your speed and endurance for an event.
Alternatively, incorrect load management is one of the greatest contributors to overuse running injuries that we see in the clinic, and it contributes to injuries such as achilles tendon problems, recurrent calf sprains, lateral hip and knee pain, shin splints, stress fractures and so many more.
As a keen runner and physiotherapist, I have had an interesting relationship with load management over the years. I have tipped the scales a little too far in either direction on numerous occasions and suffered the consequences. As a result I have learnt some great lessons: how to monitor load, listen to my body and to get the results that I strive for. You are definitely not alone, and I hope that you can learn from my mistakes!
Okay, so you’ve also suffered from an overuse injury, or are currently suffering from one… where did you possibly go wrong?
Lets think back on your running history. When your symptoms started, what was your running program like? How have things progressed or regressed since then? There are many more questions that we will need answers to, as the key to where your load management went gone slightly askew lies somewhere in the midst of all the fog.
Common scenarios that make our ears pick up include:
Returning to running after time off from an injury
Returning back to training after a month or two of holiday (how good)
Increasing intensity following a couple of weeks of illness where loads were reduced (shorter, less intense runs)
Sudden changes in training goals or race distances
A change in training surface, terrain (hills), intensity (e.g. intervals) or footwear
The weekend warrior – someone who typically doesn’t do a lot during the week but goes all out in the weekend!
Do any of the above sound vaguely familiar?
If so, lets take a leaf out of my book and do things differently from here on out...
What is the best way to monitor and manage load? You might be wondering “how do I best structure your training program to get the best results?”
There are numerous ways in which athletes and health professionals choose to manage training loads. Here are a few ideas:
The 10% rule
The 10% rule is simply not increasing your weekly training loads by more than 10% from one week to the next. It is a very simple and often effective way to ensure that your loads are not increased too quickly. You need to consider what your baseline loads are, what surfaces you are normally training on (hills, grass, road etc), and the intensity of your training, as they will affect your overall training load and therefore injury and burn-out risk. Please note that the 10% rule has significant limitations at the different ends of the spectrum of runners, such as those who run less that 15-20km per week, or over 100+km per week, but is great for its simplicity for the majority of runners.
The Acute/Chronic Workload Ratio (ACWR)
The ACWR is becoming more popular and you might see it in your current program. It takes into consideration your baseline loads, training surfaces and training intensity to ensure that you are not over or under training. It’s a bit more tedious to analyse all the data that you need to collect, however it is a great tool to predict your future injury risk based off your current levels of loading. It looks into your rate of perceived exertion (RPE) alongside the distance or duration of your run; and compares your current training week to the previous three weeks. The acute/chronic workload ratio ensures that your loads remain between safe parameters. Speak to us if you would like to know more details about the ACWR.
Lastly,
Periodisation
Periodisation is used to structure training programs which involves planning a few weeks or months in advance. I know right, its time to get organised! Periodisation is often based around an end goal for example a certain distance or time that you would like to achieve. You also need to keep an eye on your overall well-being as your mood, energy and sleep quality are vital to your success. Your physiotherapist or coach will likely throw ‘easy’ or ‘recovery’ weeks in between challenging ones.
The most successful runners have followed one of the above principles, including all of Arthur Lydiard’s athletes. Whether or not you are a weekend warrior or a seasoned ultra marathon runner you need to make sure your running loads are safe to avoid getting injured. Structuring your program with periodisation in mind will help not only with injury prevention, but other health concerns such as relative energy deficiency in sport (RED-S).
So here are my top tips for load management
Remember that load can be affected by distance or duration, intensity, recovery and training surfaces!
Do not increase your running load by more than 10% each week.
Consistency is key. Put on those shoes year round and stay active!
We are all different and hence, different training programs work best for different athletes because our capacity to adapt to mechanical stress is unique.
It is best to follow a program from someone who is aware of load management principles – have a chat to your physiotherapist or your running coach, or come and see one of our running specialists at Reload.
At Reload Physio we offer one on one running programs, strength and conditioning and recovery work. If you would like more information, or just need some reassurance with your current program please reach out.
Book a Comprehensive Running Assessment and report session (60mins), or an Initial Injury Consultation below.
Bone Stress Injuries:- Pt2
Part 2 of our Blog about Bone stress injuries. How are they diagnosed, managed and other considerations.
In our previous blog you learnt a little bit about about bony stress injuries (BSI), who are at risk and what you can do to reduce your chances of developing them. This week, we will talk about how we diagnose you with BSI and what needs to be done to get you back tracking your progress on Strava.
So, to recap, the faster you pick up a BSI the faster your recovery is likely to be. It is one of those injuries that start as a niggle, and if you do not listen to it, it can become a debilitating and long-lasting injury. Occasionally, even surgery is required to help you along!
How do we diagnose you with a stress fracture (BSI)?
During your physiotherapy assessment a thorough history will be taken. We will discuss your running program in detail, ask about your nutrition and other things, like general health, medication, stress levels, sports, work and family commitments.
After we’ve given you the third degree, we have a good look at your injury:
Palpate (touch) the area you are experiencing pain in. Bony tenderness?
Get you to hop a few times or do other specific loading tests (low evidence) especially if the area is difficult to palpate.
There is a high chance that we will refer you for imaging if we suspect that you have a bony injury. An X-ray will be done first, and if nothing shows up on X-ray but your symptoms are in an area that is considered as ‘high-risk’, or if you are still in pain after a couple of weeks, then you will be sent for an MRI.
Did you know that if you are under the age of 16 years your MRI can be bulk billed in Victoria?
A combination of your symptoms, location of your pain and imaging results would result in a diagnosis of a BSI.
I have been diagnosed with a stress fracture or BSI, now what?!
Depending on the classification of your injury we might refer you to a sports physician. If the injury is classified as ‘high-risk’ then surgery will often be recommended.
On the other hand, low-risk BSI generally heals well with modifying your activity levels and gradually returning to running once able. It is also important to address any other factors that might be putting you at risk of developing another BSI in the future. For example, managing your training load, and improving your bones’ ability to take load and correcting your running technique.
Regardless, our first aim is to have you pain free with day to day activities with the use of footwear, a brace, boot or crutches. Eliminate night pain, or pain at rest to avoid the use of pain medication and non-steroidal anti-inflammatories as they can delay healing and mask your pain.
Once that is achieved, you need to maintain your aerobic fitness – yes, you will still exercise! Safe examples include swimming with a pool buoy, deep water running (with modifications), seated cycling. All of these activities need to be pain free for them to be suitable.
At Reload Physio we will ensure the range of motion of your affected joints are not compromised and maintain muscle activation with manual therapy and home exercises. We will work on ‘imbalances’ and biomechanical contributing factors so that it is a smooth transition back to a gradual canter.
You will also be given a tailored return to loading program. It is slow and gradual and will include strength training as well as running. Generally, if you’ve had six weeks off it would take a minimum of six weeks to reload the area. Your patience is key, after all slow and steady wins the race!
Other areas that might need to be addressed include your nutrition and energy intake. A sports dietitian is an invaluable resource and your physiotherapist will refer you to the best in the business if indicated. Your use of medication (especially glucocorticoids and anticonvulsants) might need reviewing, and, in females, your menstrual cycle will need monitoring.
Moreover, it is crucial to have a good support team around you. Your family and friends, as well as a good medical team are essential to get you through the weeks where you are not training, or not training as much as before. Try to catch up with your usual running friends over a cuppa, instead of hitting the pavement!
Physio Carla Bywater is a physio with extensive experience in running, crossfit and other high load sports as both an athlete and a physio.
Bone Stress Injuries a.k.a Stress Fractures
Have you ever wondered what a Stress Fracture is? Why they occur and what to do about it? Physiotherapist Carla outlines all of the details in Part 1 of this 2 part Blog on Bone Stress Injuries.
Have you ever wondered what a Stress Fracture is? Why they occur and what to do about it? Physiotherapist Carla Bywater outlines all the details in Part 1 of this 2 part Blog on all things Bone Stress Injuries (BSI’s)
As summer is well and truly upon us, many, me included, are trying to make the most of the sunshine and extra daylight hours by heading outdoors for exercise. The amount of running trails and routes in Melbourne are endless, so needless to say, sometimes my runs end up longer than expected! As I increase my training load, I am becoming increasingly aware of the risks associated with long distance running, such as bony stress injuries.
In our official first week as Reload Physio in November, we had the privilege to listen to Dr Adam Castricum present on stress fractures and relative energy deficiency in sport (RED-S). Adam currently works at Olympic Park Sports Medicine Centre as a sport and exercise physician.
What are stress fractures?
Stress fractures are overuse bone stress injuries (BSI) that commonly result from a sudden change in training or exercise load. For example, increasing your training volume for a race or starting to train after a period of inactivity – “Hello New Year resolutions!” And in my case, I’ve decided to take my running more seriously again after giving birth to my daughter a year ago.
Why do they occur?...
Our bones are constantly remodelling based on what loads we place upon them. This is a good thing, and usually results in stronger bones. But if we do not allow enough time for our bones to rebuild and adapt after an increase in load, then BSI can develop.
BSI result from the “inability of bone to withstand repetitive mechanical loading, which results in structural fatigue and localised bone pain and tenderness”
There is a continuum of severity with BSI from mild to severe:
Yes, Bone Stress Reactions can develop into a Complete Fracture
Therefore, the earlier a BSI is detected, the better, and the quicker your recovery will be!
Who normally develops bony stress injuries?
Between one to two thirds of competitive long-distance runners or cross-country runners suffer from BSI. Other at-risk populations include competitive track-and-field athletes. Unfortunately, if you’ve suffered from a BSI, the likelihood of it happening again is relatively high (up to 12.6%).
Where do they most commonly occur?
Common injury sites include: the tibial diaphysis (shin), femur (thigh), fibula (shin), calcaneus (heel), metatarsals and tarsals (foot). Less common sites are the pelvis and lower back.
Are some worse than others?
Yes, as mentioned earlier, there is a continuum that your bone injury will fall on. To make things easier a classification system was developed. If we want to get technical, you have high or low GRADE, and high or low RISK.
High or low grade of a BSI refers to how your injury looks on imaging. Has it been present for a short time? Then it is likely a low-grade injury. Or has it been worsening over a longer time period? Which places it into the high-grade category. Classifying it into high or low grade allows us to give you an estimated recovery time. Low grade BSI tend to heal faster than high grade ones.
High or low risk refers to the location of the injury. The location is important as there are certain areas of bone that experience the most tension/load. Treatment of high-risk bone stress injuries are more difficult and require a more aggressive approach to avoid complications. For example, the BSI may develop into a complete fracture, or delayed union or non-union of the fracture site! Ouch!
If a high-risk area is involved, an experienced sports physician will become involved to carry out an orthopaedic assessment. Surgery is a real possibility to fixate the bone in order to promote healing and avoid further complications.
I bet this all seems rather daunting, but do not worry! Healing time frames vary from just under nine weeks (low risk and low-grade BSI) to 20 weeks (high-risk, high-grade). High-risk sites take longer to return to running, regardless of if they are low- or high-grade. It is very important to remember that you and Sally next to you are completely different! Therefore, your return to running timeframes will vary, so don’t try to compare your progress.
As a general rule, at Reload Physio we follow the mantra: “treat the patient not the X-ray”.
“But why do some runners develop a BSI and others not?” You might ask, especially if a similar amount of distance is covered each week.
The answer is multifactorial. Some things are within your control, while others are not. For example, things such as genetics and bone diseases are bad luck and you are not able to change them. While it is easy to focus on the dire, there are other things you can do, or not do, to reduce your chances of developing a BSI.
Because bones are living tissue they respond, and adapt, to the load that is placed upon them. Your running technique influences the amount and direction of force that passes through your bones. If you think your running technique can use some fine tuning it is super easy to get a running analysis done, and to go home with a few things to work on.
Your running program (or lack of) can have a huge impact on your risk of developing a BSI. Have you recently started running from scratch, or increased your running pace, duration or frequency? A significant change in load management is central to disrupting the fine balance between bone ‘building and breakdown’ that occurs on a day to day basis.
Other things we need to think about: your footwear and running surface (trail vs road, or treadmill to pounding the pavements). Neither have been proven to have a direct causal relationship to BSI, however, if either has been changed recently and you have developed bony tenderness, then it is worth looking at as contributing factors!
To reduce your chances of developing a BSI you need to consider the following ‘gems’:
Stay active life long, and encourage your children to do the same, because a longer history of physical activity is thought to be protective against BSI.
Strength training: add this bad boy to your training program to get your muscles stronger to help your bones to absorb ground reaction forces during running. Weaker muscles do not absorb the ‘shock’ as readily and fatigues faster, influencing your technique too!
Nutrition: firstly, you need enough fuel to sustain your training load to avoid a relative energy deficiency. Secondly, your body needs adequate levels of vitamin D and calcium in your diet to support bone health. If we think that this is a contributing factor to your BSI, we will refer you to a dietitian to get the best guidance.
Your hormone and endocrine function are closely related to your energy intake and expenditure. To learn more about relative energy deficiency in sport (RED-S) read our previous blog here.
Avoid sudden changes in loading! If unsure, get professional guidance.
Did you know at Reload Physio we offer comprehensive running analysis, coaching, running technique training as well as movement and strength and conditioning classes to get you back to where you need to be in the future?
Click below to book in for a thorough running assessment by one of our running specialist physiotherapists.
If you feel you may need your running assessed, a training program developed, or need a personalised exercise program to work on your weaknesses, then we have you covered.
If you are recovering from a running related Bone Stress Injury we recommend booking in for a Comprehensive Running Assessment with one of our Physios.
RED-S
Relative Energy Deficiency in Sport
Our Physiotherapist, Carla Bywater, delves into RED-S, a common, but often undiagnosed contributor to bony injuries, performance plateaus and other more serious complications for athletes who are pushing their body to its limits.
Relative Energy Deficiency in Sport
Do you have to ‘make weight’ for your sport? Are you in a very physically demanding job? Have you increased your training load? If so, you need to be aware of the risks associated with “Relative Energy Deficiency in Sport” (‘RED-“S” or “REDS”).
What is RED-S?
You might be familiar with the term ‘the female athlete triad’, which is a classification system used to identify female athletes who suffer from athletic amenorrhoea (loss of their monthly period), osteoporosis (weaker bones) and eating disorders.
In 2014 the female athlete triad was ‘upgraded’ to RED-S to recognise the fact that both males and females, young and old are affected by it. Furthermore, it identified widespread and long-term health effects and a reduction in performance in those affected by RED-S.
The basic principle of RED-S is low energy availability. In other words, an athlete is not consuming enough energy through their diet to sustain their training load as well as day-to-day living.
Just to ‘be’ requires energy and fuel. The athlete’s normal physiological processes such as bone health, hormone production, reproductive health and the immune system get placed on the ‘less important’ list as the athlete’s body is essentially in starvation mode.
Why would their body use energy to maintain their ability to reproduce if there is not enough food going around?
RED-S is defined as: “impaired physiological functioning caused by relative energy deficiency and includes, but is not limited to, impairments of metabolic rate, menstrual function, bone health, immunity, protein synthesis and cardiovascular health”
Sporting codes that have a high prevalence of RED-S include running, triathlon, cycling and dancing. In the past, it was favourable to lose weight in order to ‘go faster’, ‘jump higher’, be easier in ‘point’ if you were lighter. Unfortunately, the long term health effects of a sustained energy deficit are becoming more and more apparent in recent years.
RED-S is a continuum from mild, moderate to severe. Therefore, the earlier it is addressed, the better.
Common signs that you might be suffering from low energy:
Have you noticed a declined in performance? Are you unable to sustain high-intensity efforts like you used to? Taking longer to recover after training? Waking up tired in the morning? Suffering from body soreness?
Females – have you had any changes with your monthly cycle, especially if you have not had your period for six months or more? Males – have you noticed a decline in your sex-drive?
Have you had reoccurring colds, coughs or upper respiratory tract infections? Have you suffered from stress fractures in the past? Have you been diagnosed with low iron?
Are you relatively strict with what you should or should not eat? How do you feel if you miss a training session (anxious/angry or frustrated, or do you accept your circumstances)?
It is essential to identify low energy availability as soon as possible to minimise the impact on your health and performance.
As an athlete, you might not be too concerned about your immune status or your ability to reproduce. What if I told you that RED-S has a significant impact on your ability to perform at your best, that it could be the one thing that is holding you back?
Performance consequences of RED-S
Decreased muscle strength
Decreased endurance performance
Increased injury risk
Decreased training response
Impaired judgement
Reduced coordination
Reduced concentration
Irritability
Depression
Depleted glycogen stores
If the above does not motivate you to seek treatment to improve your athletic ability, then I am not sure what will!
How do we treat an athlete who’s suffering from RED-S?
The treatment of RED-S requires an interdisciplinary team approach. Often a sports medicine doctor, dietitian, physiotherapist and psychologist are involved in getting the best outcome for the individual.
It is crucial to regain the balance between the athlete’s ‘energy in and energy out’; to restore their morning energy levels, regain regular menstrual cycles (females), return homeostasis to oestrogen and testosterone levels, alongside a graduated return to exercise.
Sounds simple right?
Please note – the oral contraceptive pill is NOT the answer to restore the athlete’s period.
If you would like further information, please do not hesitate to talk to one of the physiotherapists here at Reload Physio or do further reading. The following links offer great insight to both athletes, parents and coaches:
Ask a Physio:- I'm keen to start trail running, what should I be careful with?
Our Principal Physio, Marcus, shares some important tips so you can enjoy running in the trails this summer.
Author:- Marcus Pain, Principal Physios and keen runner.
Trail Runner Magazine Aug/Sept 2017
Trail running is like the Rally sport of Motor Racing or the mountain biking of cycling, it is a fantastic alternative to running through the concrete jungles that many of us live in. But just like rallying and mountain biking, the risks are very different to the road alternatives. Try visualising a Formula 1 car doing the jumps like a rally car, or riding a Tri Bike down a dirty big mountain (offroad), I’m pretty sure neither would end well. With trail running there are many key differences that we must consider and prepare ourselves for, and from my clinical and practical experience, being informed is the critical first stage of injury prevention in this great sport.
All types of running, in fact almost all types of sport, have injury risks. Injuries in road running, like many endurance sports, are largely attributed to repetitive overuse injuries. Trail running has many similarities to road running, but there are many differences between road and trail running and some of these are much more obvious than others.
So, what should you be careful with? We could go in many directions with this question, such as getting lost, knowing the terrain that you are going to, the wildlife, especially the slithery type, and the first aid that goes along with these... but for this article I will stick to the physiotherapy side aspect, ie the injuries, we will cover the likely causes and will give you some general tips on what you can do to minimise the risks as you start.
The information provided here is important for all newcomers to trail running, whether already an experienced road runner, or a novice runner. In my clinical experience, it is often the roadies that suffer many injuries when they hit the trails, probably because it is not their cardiovascular fitness holding them back, but it is that their body is not prepared for the new conditions. One example is a friend who o is a 90minute half marathoner, he joined me for a trail session in the hills surrounding Melbourne for ‘something different’, we covered about 20kms at a cruisy pace over 2.5 hrs, and he was generally sore for days and it set off his Plantar Fasciitis.
The varied nature of trail running reduces the occurrence of the repetitive overuse running injuries, and in many cases I recommend injured runners incorporate off-road running as part of their return to running rehab because the loads on the body differ with each and every step, and this variety of load means that many different structures are sharing the strain rather than the same each step, there is less repetition. But there are things to be careful of, some more obvious than others. These I will simplistically classified under two categories, the acute injury and the load related injury.
Firstly the obvious, the acute injury...
Falls, Twists and Sprains
The uneven terrain on the trails means an increased risk of twists and sprains, any misplaced step can result in ‘going over’ on your ankle, or slips and falls resulting in bruises and impact injuries. As a newcomer to trail running an immediate difference you will notice is the need to watch the path ahead each and every step. Learning where to step, what surface is stable, what will move underfoot, how heavy is safe to land, and even simply how big your foot all takes time and practice, and they are things that rarely need to be considered when road running. Part of preventing these injuries comes down to proprioception, a key factor of balance, this is your own body’s sense of joint movement and position in space, more simply, do you know where your joint is? And, how quickly are you aware of any change in position? Proprioception, foot-eye coordination, strength, balance and stability are all very important to staying on your feet. If you have ever seen a top trail runner descending a steep, technical terrain, they are amazing, they have incredibly fast feet, every foot placement is perfect, they have great stability and it looks easy. This skill takes time, practice and experience. Be patient, it will come.
Now the load related injuries:-
When we think of trail running, we immediately think of the hills and the challenges attributed to them, the newbie will typically moan and groan at the thought of climbing the steep inclines, however, the climbing is not what will cause the groans the next day!
The bit you think is easy… is the hard bit on your body, the downhill.
Many running injuries are cause by load, and ‘flying down a hill’ is were load is at its greatest. The degree of decline is a huge factor here. The angle where a relaxed run down hill is now an effort, where you feel that relaxing isn’t possible as doing so will result in just going faster and faster until you lose control, this is where your body starts to whimper, the impact is high, and so are the loads. Your knees, quads (thighs), hips, they all feel the impact. This ‘putting on the brakes’ is where you are eccentrically loading your muscles, where they are working hard as they lengthen. This impact and eccentric loading causes that familiar day-after hobbling and cursing of every minor decline or flight of stairs that you never previously noticed. When your body is not conditioned to this impact and eccentric loading, it hurts, so gentle exposure and graduated loading over a period of time is the solution.
Another factor when it comes to downhill technique is that newcomers don’t immediately have the foot-eye coordination to have fast feet downhill, their risk of tripping is very high, so the tendency is to take long lunging steps, this allows more time to look and plan your next step, the bad news with this approach is that this magnifies the load even further, and the risk of twists and sprains. Once coordination improves, running downhill should be about fast, light feet, minimising impact and jarring, this reduces the load on your legs, causing less injuries and the bonus is that it will result in greater endurance.
So what can you do?
Three things, and ideally all three, especially number 3!
1. spend a bit of time planning where you are going, initially don’t try and climb Mt Everest if you usually run on the flat, use online platforms such as www.movescount.com to find a route that is gently undulating rather than all steep ups and downs, find areas that are not too rocky or covered in tree roots.
2. take it slow to start with, don’t push yourself, monitor your loads and don’t be a hero. Week by week gently progress as your body gets conditioned to your newfound love of this sport. Keep the distance well within your comfort and enjoy the day. Listen to your body and seek help from a Physio if any niggles develop.
3. This takes more work, but in my view, is a critical component, it will get you to achieve more, quicker, and aims to bulletproof you from injury, it involves specific exercises that strengthen your weaknesses, improve your balance and proprioception, your foot- eye coordination. The exercise program should involve exercises that target all the leg muscles, from your calves to gluts, as well as your core region and must include balance, proprioception and agility exercises, concentric and eccentric exercises. Speak to a Physio or trainer who knows the sport and can write a program that targets your specific weaknesses while being specific to trail running, ideally someone with experience in the trails themselves.
Also:- Footwear:
It is preferable to have specific trail shoes too, they have much greater grip, more lateral support to tolerate the side to side movement of trail running. Road shoes are primarily designed to go forwards. In my opinion, and I am sure I am not alone on this, one of the most fun parts of trail running a narrow single trail that winds side to side, and without appropriate shoes there will be greater risk of slipping sideways or rolling an ankle. So, save your road shoes for the road, spend a few dollars and get kitted out for he trails, and besides who doesn’t like a new pair of shoes… covered in mud?
Recommendations for trail newbies:-
1. don’t be a hero, your fitness may not be your limiting factor, it may be your ability to stay on your feet.
2. Initially choose gentle non-technical trails
3. Minimise distraction so you can focus on the trail ahead, this may mean no ipod, or not as much chatting on some parts of the run, enjoy the sounds of nature.
4. Bulletproof yourself
5. Have appropriate footwear
First published in Aus TrailRunner Magazine Aug/Sept 2017
Marcus has completed many trail run in Victoria, interstate and overseas- his greatest personal trail running achievements include the UTA100 (Blue Mountains- under 13hrs), Bogong To Hotham 56km, Tarawera 85km Ultra- NZ.